Stefan Trines, Research Editor, WENR
Late last year a gathering of international health professionals in Dublin discussed the steps necessary to head off a projected shortfall of 18 million healthcare workers worldwide by 2030 [2]. As alarming as that statistic is, it is a bellwether for the future strength of nursing and other health occupations.
Nursing is one of the fastest-growing occupations in the U.S. — the Bureau of Labor Statistics anticipates that 438,100 new jobs [3] for registered nurses will be created in the U.S. by 2026. To fill many of these jobs, it might be necessary to hire more foreign-born nurses, which in 2016 already held about 15 percent [4] of all registered nursing positions.
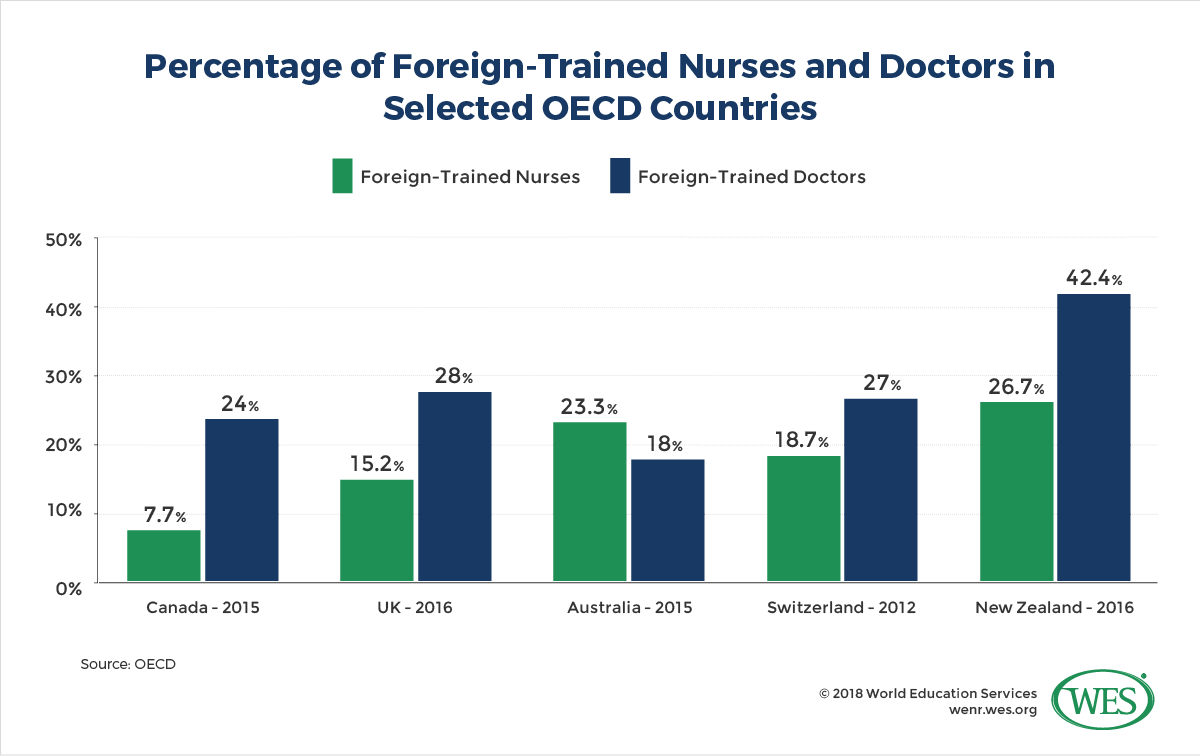
In other countries that percentage is even higher: 18.2 percent [5] of nurses in Australia were foreign-trained in 2016 (up from 14 percent in 2009), compared to 26.7 percent in New Zealand (up from 14.7 percent in 2002). In the Arab monarchies of the Gulf Cooperation Council (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates), the share of foreign nurses was as high as 79 percent [6] in 2008.
These numbers reflect that the international labor migration of nurses and other health workers is on the rise worldwide. As the WHO and the Migration Policy Institute have noted [8], “existing shortages and inequitable distribution of the health workforce” have led to an “expansion in the international migration of health workers, with patterns of migration becoming increasingly complex.” Developed countries “have become more … reliant on international migrants to fill health workforce positions…, from home health aides …. to nurses, physicians, and medical specialists”. This dependency “is expected to continue in coming decades and – in several health occupations – intensify.”
In this article, we will look at trends in nurse migration within the context of international labor migration as well as how the looming healthcare worker shortage is already playing out around the world. Then we will look at international mobility patterns and some of the forces that are driving mobility in the sector. The Philippines and (increasingly) India are major sending countries of international healthcare workers, so we will examine these countries in greater detail and also discuss the impact labor migration has on the health care and education systems of source countries.
Nurse Migration Trends
Current trends in nurse migration do not always follow a linear growth trajectory and can be difficult to measure since not all governments provide reliable demographic and employment statistics. Macroeconomic factors, such as the 2008 global economic crisis, affect migration rates, as do changes in immigration policies, particularly in countries that use temporary work visas to remedy cyclical labor shortages on a short-term basis. Despite an overall increase in the labor migration of nurses worldwide, migration rates of nurses have consequently ebbed and flowed over the years and vary strongly by country.
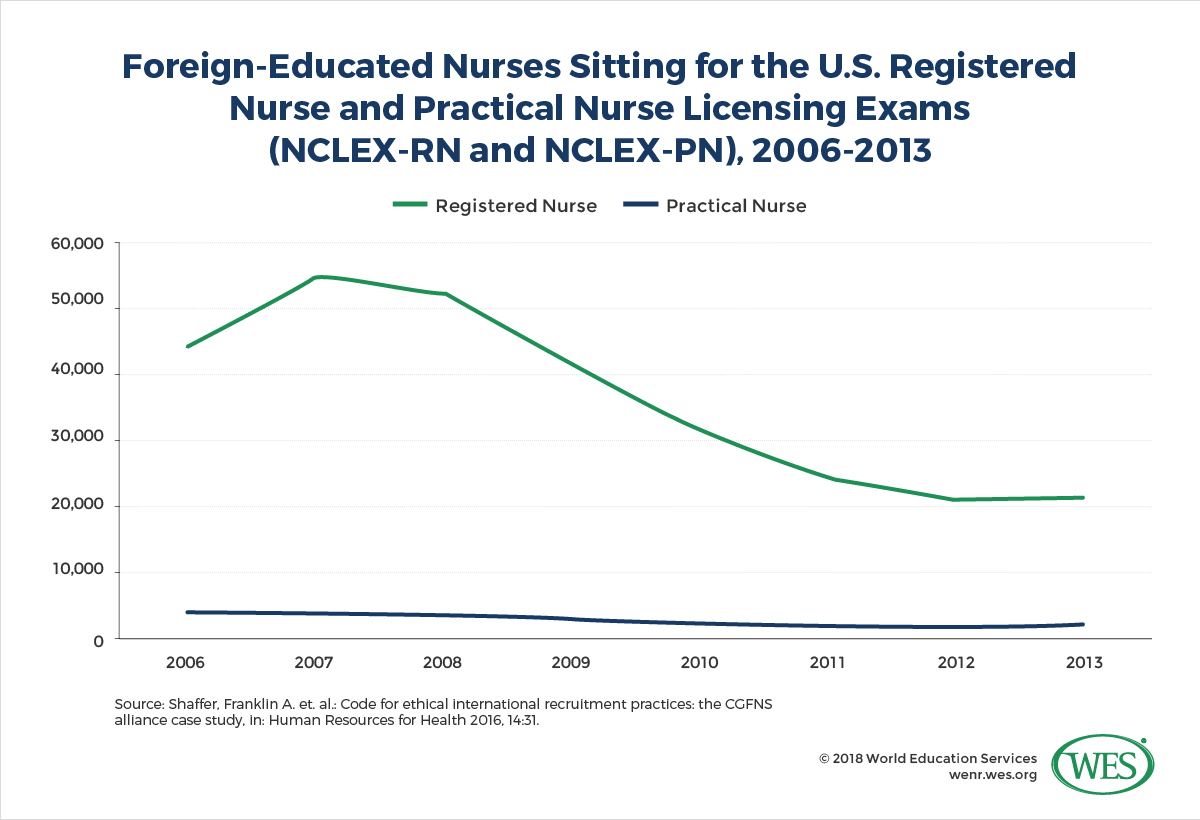
In the U.S., for example, the annual inflow of foreign-educated nurses has decreased pointedly [9] over the past decade after peaking in 2007. The importation of nurses has become an increasingly controversial political issue in recent years. Former U.S. President Barack Obama in 2009 already resisted lawmaker’s attempts to create new work visa categories for foreign nurses, noting [10] that the “…notion that we would have to import nurses makes absolutely no sense. There are a lot of people (in the U.S.) who would love to be in that … profession, and yet we just aren’t providing the resources to get them trained—that’s something that we’ve got to fix”.
As a result, the options for foreign nurses from non-NAFTA countries to work in the U.S. are presently more restricted than in the past. U.S. employers can sponsor a limited number of registered nurses (RN) for permanent residency under the EB-3 immigrant visa [11] for shortage occupations – an extensive process with very long wait times. Foreign nurses may also enter the U.S. on H-1B visas, even though that visa category is for positions that require at least a bachelor’s degree and therefore limited to advanced nursing positions, such as nurse practitioners or nurse supervisors. (The minimum educational licensing requirement [12] for registered nurses in most U.S. states is still an associate degree, despite a trend [13] towards requiring [14] a bachelor’s degree).
Under the Trump administration, the prospects for the recruitment of foreign nurses remain uncertain. Potential future restrictions on H1-B visas could impede the inflow of highly skilled nurses. The possibility of far-reaching changes to the NAFTA treaty, meanwhile, could curtail the labor migration of RNs from Canada and Mexico, which can currently work temporarily in the U.S. on TN work visas [15]. The travel ban on Muslim-majority countries will bar health professionals from affected countries from entering the U.S., thereby eroding the country’s stock [16] of doctors and other health workers.
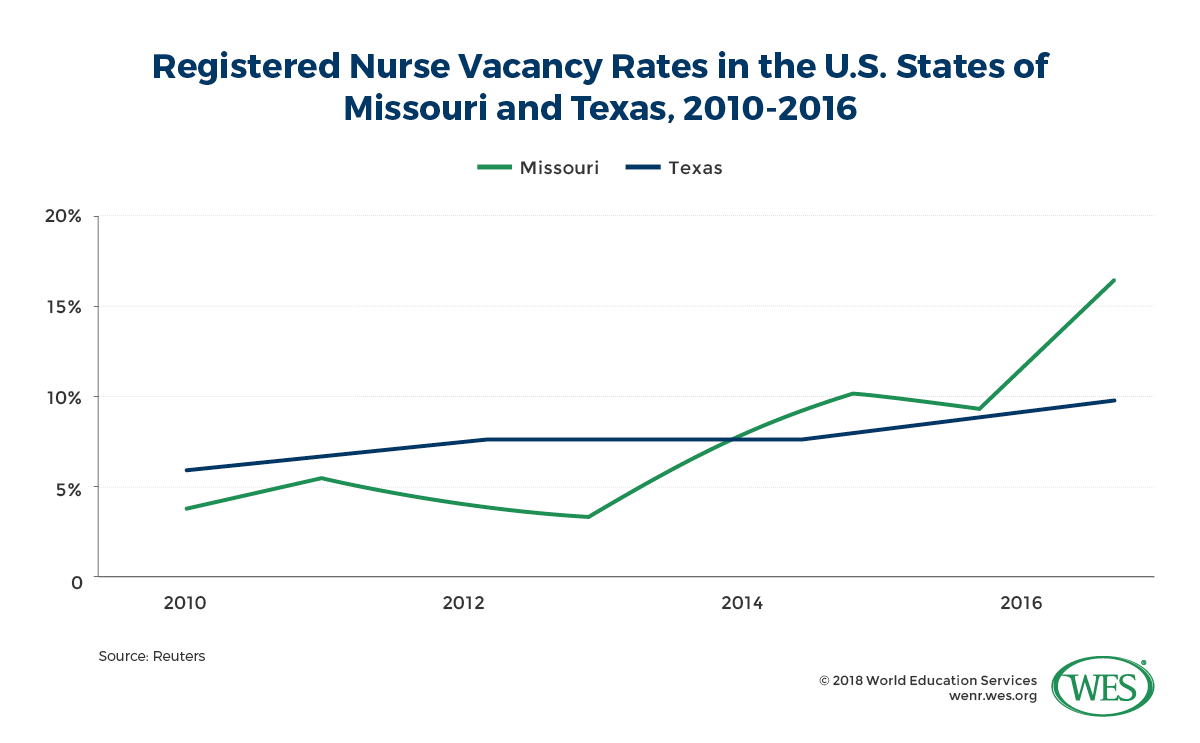
At the same time, an acute shortage of nurses in the U.S., coupled with the failure of the U.S. system to boost the supply of nurses domestically adequately, creates a strong incentive to recruit more foreign-educated nurses. In 2017, hospitals throughout the U.S [17]. already struggled to fill nursing positions and collectively spent billions of dollars on the recruitment and retention of nurses – a circumstance that has caused Congress to open the doors to foreign nurses in the past. It, therefore, remains to be seen if the anti-immigration impulses of the current administration will hold up under acute economic pressures to import much needed skilled labor in the health sector.
The Global Backdrop: Growth of International Labor Migration
On a global scale, the growing cross-border mobility of nurses and other health workers comes amidst advances in international labor migration in general. Over the past decades, increasing numbers of economic migrants have sought better career opportunities, higher pay and an improved quality of life by pursuing employment abroad. According to the latest available estimates by the International Labour Organization (ILO), the number of international migrant workers has tripled since 1990 and stood at 150.3 million in 2013 [19].
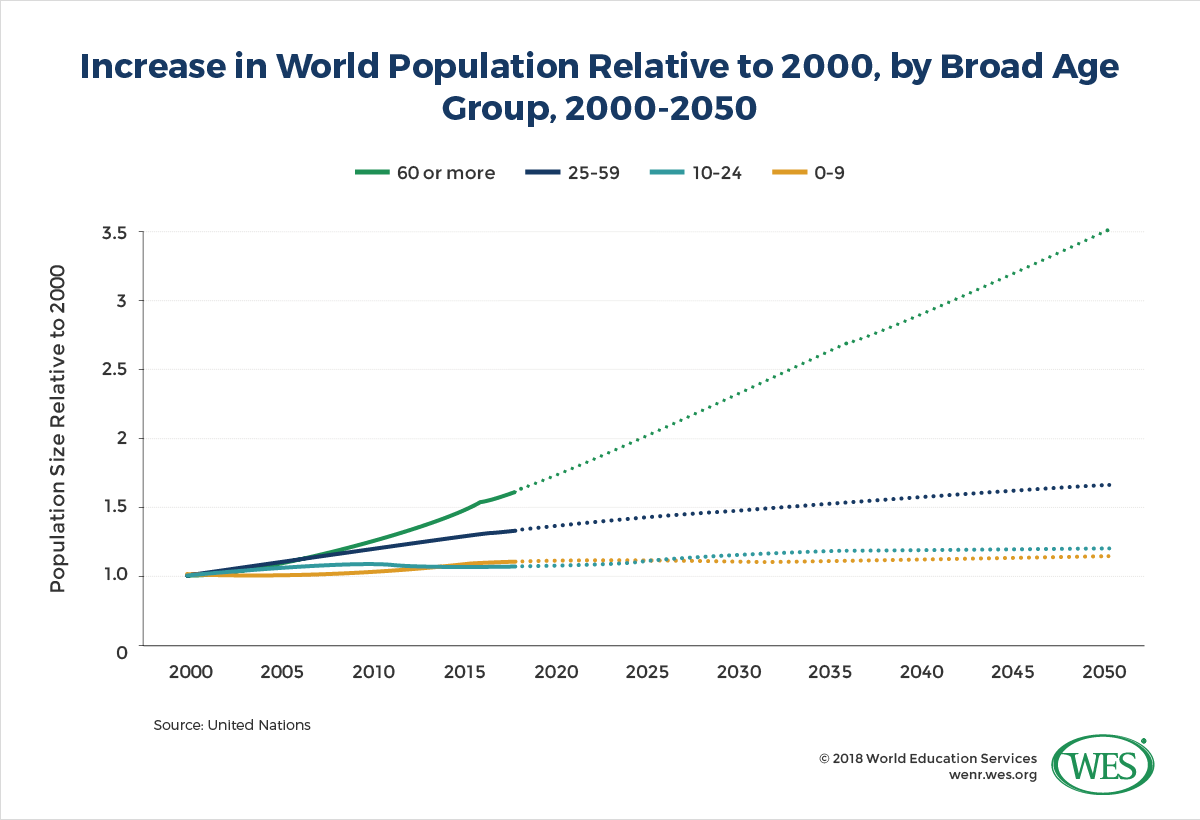
Contemporary labor migration is concentrated in the service sector and often from less developed countries to richer world regions. According to the ILO, the vast majority of mobile workers move to high-income countries, with North America and Western Europe alone hosting almost half of all migrant workers worldwide (48.5 percent [19]). The world’s two largest migration corridors [20] in 2015 were between Mexico and the U.S. and between India and the United Arab Emirates, where Indians now make up more than a quarter of the population. Population aging and the shrinkage of labor forces in high-income countries are pull factors that will likely sustain this movement from the “global south” to the “global north,” despite governments in some Western countries currently seeking to curb immigration levels.
Push factors in sending countries will further drive the trend: while the number of people above the age of 60 is anticipated to increase by 23 percent [21] in developed countries by 2030, this graying of higher income societies is paired with rapid population growth and exploding youth populations in many developing countries. Faced with poverty and limited employment opportunities, the burgeoning youth population in Sub-Saharan Africa, South Asia, parts of the Middle East, and other regions of the developing world will provide a growing pool of potential migrant labor.
But labor mobility is anything but limited to south-north migration. Advances in communication technology, the ease of travel, trade liberalization, the removal of international employment barriers and the harmonization of education systems in regions like the European Union have contributed to increases in labor migration in various directions, including accelerated north-north migration. Citizens of other EU countries, for instance, make up about half [22] of all migrants in the European Union. South-south labor migration between low-income countries has also expanded [23] and is expected to further grow in volume in the future [24].
Worldwide Shortage of Nurses
Nurses and other health professionals provide vital in-high-demand services in virtually all societies and are among the groups of workers likely to continue to migrate internationally in high numbers. At present, there is an acute global shortage of health workers that is unlikely to dissipate in the near term. Nursing shortages are not new and have plagued countries to varying degrees before. The demand and supply of nurses in the U.S., for example, have fluctuated [25] strongly in previous years. The recent crisis, however, appears to be a longer-term problem on a global scale.
Current estimates [26] suggest that 40 million new health sector jobs will be created until 2030 worldwide, but that there will be a lack of 18 million health workers [27] to fill these positions. Nurses and midwives are among the health professionals for which demand outstrips supply. The WHO estimates that there is presently a shortage of 9 million nurses and midwives [28] worldwide – a gap that is expected to narrow only slightly to 7.6 million by 2030.
Population aging is one of the most pressing drivers of demand for nurses and other healthcare professionals. The UN estimates [30] that the number of people above the age of 80 will more than triple until the middle of the century, from 125 million in 2015 to 434 million in 2050. These people, the so-called “oldest old,” will live longer than ever before and require increasingly complex medical care.
Population aging is presently mainly a problem of high-income countries, with Japan, Germany, and Italy being the most aged countries [21] (2015). But less developed world regions are anticipated to become increasingly affected as well: “Within the next 15 years, several upper-middle-income countries are projected to become as aged as many of today’s high-income countries. Between 2015 and 2030, the share of population aged 60 years or over is projected to increase from 15 percent to 24 percent in China, from 20 percent to 32 percent in Cuba, and from 16 percent to 27 percent in Thailand”.1 [31]
There is little doubt about the severity of the problem. Fast-aging China, a country where 40 percent [21] of the population is projected to be above the age of 60 by 2050, for instance, already grapples with a shortage of nurses in the millions. In 2012, China had only 1.8 nurses per 1,000 people [32], compared to an average of 8.8 nurses per 1,000 people in the OECD. Care for the elderly is now said to be in a state of crisis [33], with observers polemicizing that the wait time for a slot at a nursing home in Beijing amounted to 100 years [34] in 2013. In Japan, the oldest country in the world, meanwhile, the government is increasingly investing in the development of nursing care robots [35] to help cope with an expected shortage of 380,000 health nurses [36] by 2025.
A closely related problem is the aging and erosion of the RN workforce in several countries due to retirement. In the U.S., for example, approximately 1 million out of 2.86 million [38] RNs (2016) are “over 50 years of age, and it is expected that “one-third of today’s nursing workforce will reach retirement age within 10 to 15 years [39]”. In the UK, likewise, one in three [40] nurses is expected to retire until 2026.
Other factors that facilitate the global nursing shortage include:
- Decreased interest in nursing as a career choice and insufficient numbers of nursing graduates in some countries.
- Attrition of the nursing workforce due to poor working conditions, the slashing of health budgets and inadequate funding of hospitals.
- Gender bias that denigrates nursing as a “female profession” and keeps greater numbers of males from entering the profession in some countries (in the U.S. the female-to-male ratio among nurses was 5 to 1 in 2015 [41]).
- Increased participation of women in the labor force, creating a greater need for paid professional care of the elderly and other household members.
- Rising income levels and increased access to healthcare.
The most severe shortages of nurses, however, are found in poor developing countries. Because of a lack of critical resources, the health care systems in many of these countries are in a state of crisis, including a very low ratio of nurses to the overall population. “Globally, health workforce shortages continue to be greatest in sub-Saharan African countries that together bear 24 percent of the world’s disease burden today, but have only 3 percent of health workers and less than 1 percent of the world’s financial resources to respond to this burden [8]”. The accelerating outmigration of nurses and other health workers to high-income economies further erodes the health labor force in many countries (see the section below on “impact on source countries”).
The Pull of Higher Pay: Destination Countries of Mobile Nurses
High-income countries are in a privileged position that allows them to balance domestic nursing shortages with migrant workers, at least partially. Countries that have imported sizeable numbers of migrant nurses over the past decade include the U.S., Australia, Canada, Saudi Arabia, the U.K., Norway, Ireland, Switzerland and other European countries, with the U.S. continuing to host the highest number of foreign-born nurses worldwide (there were an estimated 1.106,565 [42] foreign-born RNs, licensed practical and vocational nurses, and nursing, psychiatric, and home health aides in the U.S. in 2015).
The stock of foreign-trained nurses in other OECD countries stood at 105,811 in the UK in 2016, 65,000 in Germany (2015) and 51,438 in Australia (2016). The number of foreign-trained nurses in Canada doubled from 14,187 in 2000 to in 30,184 in 2015, according to the OECD [9].
Unsurprisingly, the comparatively high salaries in developed countries act as a pull factor for nurses from around the world. A common salary for an RN in the U.S. is USD $68,450 [43] (median salary in 2016), and USD $51,560 [44] in Australia (2017 average), whereas the official annual entry-level salary for public sector nurses in the Philippines stood at USD $4,440 [45] in 2016. Beyond monetary gains, better working conditions, professional development, and growth opportunities are other factors that motivate nurses to relocate.
Some countries also have governmental recruitment strategies for nurses in place. Ireland’s National Health Service, for instance, in 2017 started to hold annual recruitment fairs for nurses and midwives and is offering RNs a tax-free relocation payment of USD$ 1,800 [46]. Germany recently entered formal agreements with China [47] and a variety of other countries [48] to train and integrate foreign nurses to overcome domestic shortages – an objective facilitated by the fact that a Chinese nurse can earn almost ten times [49] as much in Germany than in China.
The aggressive recruiting of nurses and other health workers from South Africa by private Western healthcare associations, meanwhile, has been likened to virtual “poaching [50]” campaigns, involving large-scale advertising drives and relocation incentives like paid airfare. The UK government felt compelled in 2005 to impose ethical standards [51] for recruitment agencies, including a ban on the recruitment of temporary nursing workers. In the U.S. alone, the number of recruitment agencies recruiting nurses abroad reportedly grew from 30 to 40 in the late 1990s to at least 267 in the late 2000s [52].
Several countries have tailored their immigration policies to promote the inflow of foreign nurses. The U.S., for example, in 1989 passed the “Nursing Immigration Relief Act” creating the H1-A visa [53] category, specifically to import temporary nursing workers to alleviate domestic shortages (the program expired in 1997). The demand for nurses in the Canadian province of Quebec, meanwhile, was so high in 2013 that the government awarded qualified nurses the highest number of points [54] in its points-based skilled worker immigration program, ahead of computer engineers and civil engineers. Japan in 2016 passed legislation that will make it easier for foreign nursing students to stay in Japan for work after graduation [55].
Countries of Origin
The labor migration of nurses is not simply a migratory movement from less developed to high-income countries. Canada is major sending country of nurses to the U.S. and there is a considerable degree of nurse migration between other developed countries, for example from Germany to Switzerland, or from the U.K. to Australia, where British nurses made up the largest share (28 percent) of foreign-trained nurses in 2016 (OECD) [5]. For every two nurses that migrated to work in the UK in 2008, one British nurse reportedly [50] migrated to the United States.
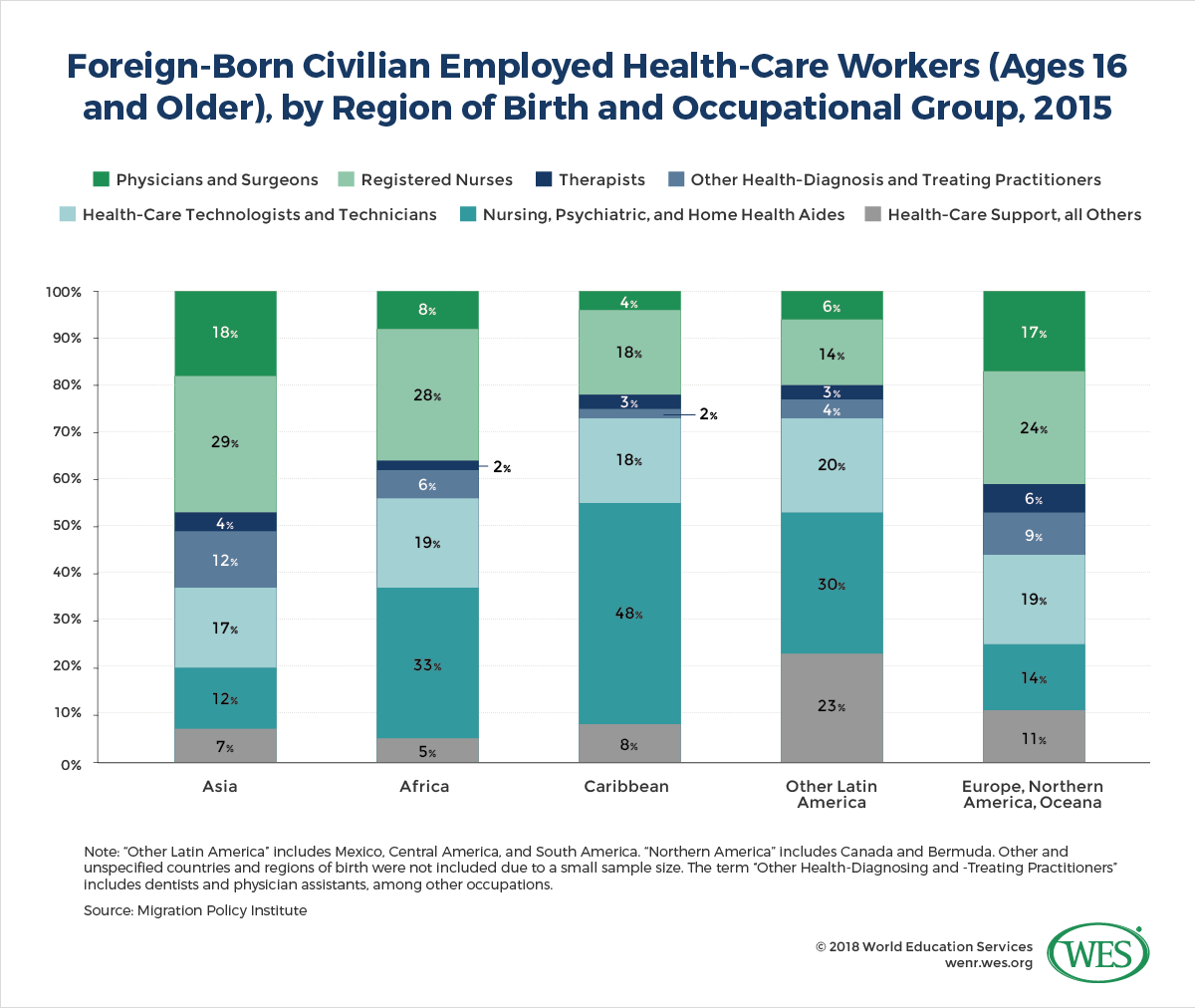
Many mobile nurses, however, migrate from middle-income countries like the Philippines India, Nigeria, or Ukraine to richer countries in North America, Europe, and the Persian Gulf region. This trend is reflected by the countries of origin of foreign nurses in the U.S.: 76 percent [56] of foreign-born RNs in the U.S. in 2015 were from Asia, Africa, Latin America, and the Caribbean, compared to only 24 percent from Canada and Europe.
“Immigrants from the Philippines accounted for nearly 30 percent of the 486,000 immigrants working as registered nurses, followed by those from India (6 percent) and Nigeria (5 percent)”.2 [57] There are also sizeable numbers of nurses from Mexico, Jamaica, and Haiti in the United States. In the U.K., similarly, the two top countries of origin in 2016 were the Philippines (23,334 nurses [5]) and India (16,931 nurses), accounting for close to 40 percent of all foreign-trained nurses combined.
 [58]
[58]
The Philippines: The World’s Main Exporter of Nurses
The Philippines has been the world’s preeminent source country of migrant nurses for decades. Starting in the 1960s, the Philippine government created a systematic, state-sponsored system of labor exportation designed to foster economic development [59] through remittances from overseas workers. Nurses played a central role in that strategy and were encouraged to emigrate. The number of nursing schools in the Philippines jumped from 17 in 1950 to 88 in 1974, and further increased from 198 in 1998 and 370 in 2005 [50], producing a growing supply of nurses. By the end of the 20th century, an estimated 250,000 nurses [59] were employed overseas in 31 countries around the world. The pull of high salaries for nurses in high-income countries was so strong that many poorly paid Filipino medical doctors, particularly in rural regions, began in the early 2000s to retrain as nurses [59] to emigrate.
Initially, Filipino nurses migrated predominantly to the U.S., mostly to coastal cities [60] – in New York City, for instance, almost one in five RNs was said to hail from the Philippines at the beginning of the 2000s. Large-scale migration to the United States was facilitated by established migration corridors, good political relations between the U.S. and its former colony, favorable immigration schemes, as well as the fact that English-language nursing training in 4-year Bachelor programs prepares Filipino nurses well for work in the United States.
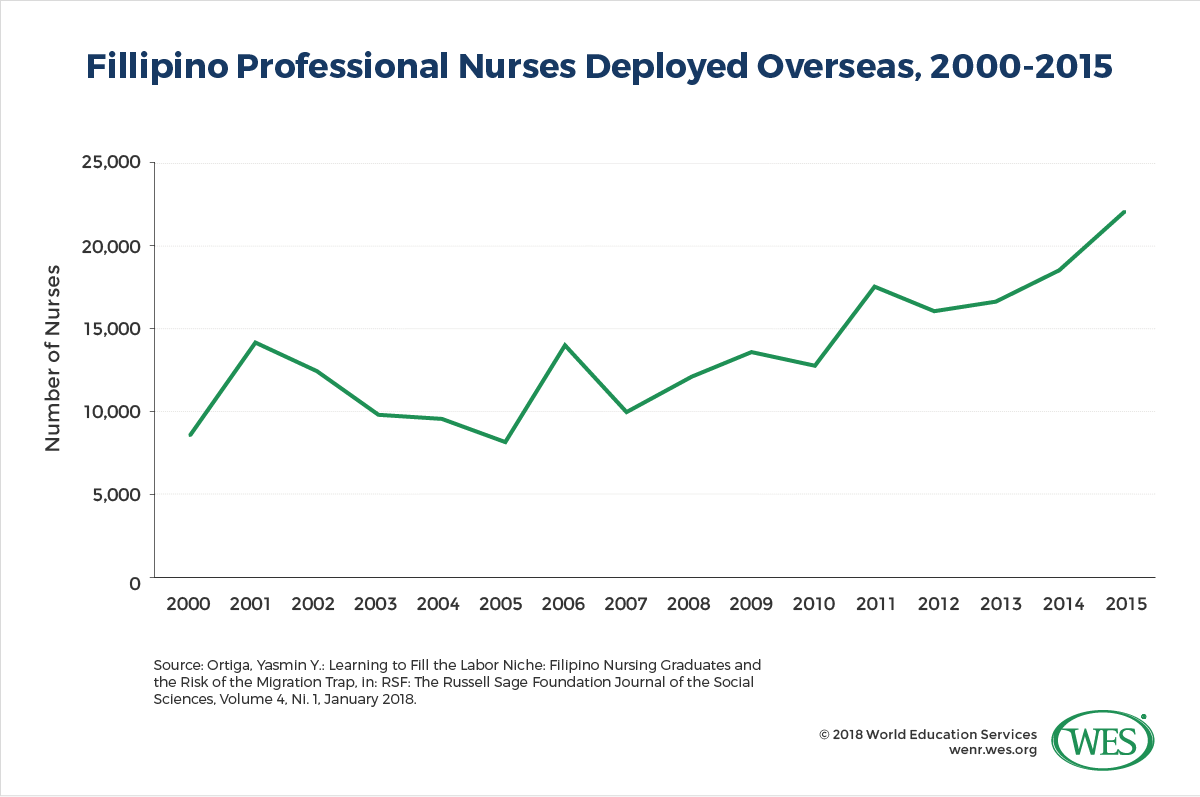
Recently, however, nurse migration from the “empire of care [61]” is increasing to Middle Eastern and Asian countries. Between “1993 and 2010 most nurses went to Saudi Arabia (90,382), 15,701 followed to the United Kingdom, and 14,895 to the United States. More current trends show that Singapore and the United Arab Emirates have been major recipients in more recent years [8]”. Migration rates also have accelerated over the past decade. According to the Philippine Overseas Employment Agency, 19,815 nurses out-migrated in 2014 [62]. The top three destination countries of all Filipino migrant workers combined in that year (excluding seafarers) were: Saudi Arabia, the United Arab Emirates, and Singapore.
India: A Growing Source Country
India, in particular, the southern state of Kerala, is another top supplier of migrant nurses worldwide. Surveys have shown that Indian migrant nurses, like their counterparts in other countries, are motivated to emigrate by better income prospects abroad, where they can easily earn ten times as much as at home, as well as poor working conditions in India [64]. The trend is also facilitated by an increase in the supply of nurses: “Between 2004 and 2010, the number of institutions offering B.Sc. nursing grew six times and institutions offering General Nursing and Midwifery (GNM) diploma courses grew by three times [65].” By some estimates, as many as 20 to 50 percent [66] of India’s growing pool of nursing graduates seek to emigrate. Despite a pronounced shortage of nurses in India itself, fully 65 to 70 percent of the approximately 10,000 nurses registering annually in the state of Bangalore alone went abroad in the late 2000s, according to the Times of India [67].
Compared to the Philippines, the labor emigration of nurses in India has historically been less systematically promoted by the government but was primarily funneled through private agencies [68] in recruitment hubs like Delhi, Cochin, and Bangalore. While reliable, current statistics on the outmigration of nurses from India are not available, outmigration is growing and has increasingly shifted from the Persian Gulf region to OECD countries [65], where Indians now are one of the top nationalities among foreign-educated nurses. Remittances from overseas Indian workers, an indicator of labor outmigration, have nearly doubled between 2007 and 2016, causing India to overtake China as the largest recipient of remittances worldwide, with a total volume of USD $62.7 billion [69].
Remittances and Brain Drain: Impact in the Countries of Origin
Remittances from citizens employed overseas can have a number of positive effects on source countries. In the Philippines, for example, foreign remittances are vital to the economy – they are the country’s largest source of foreign currency and ensure a steady infusion of funds that spur domestic consumption. In 2016, cash remittances in the Philippines reached a record high of USD $26.9 billion in 2016 [70] or about 8.8 percent [71] of the country’s GDP. Studies have shown that remittances help decrease poverty rates, particularly in poorer rural regions. The UN has noted [69] that remittances to developing nations are vital in helping these countries achieve UN sustainable development goals.
Another potential benefit of labor migration is the “brain recirculation” that occurs when labor migrants return and apply their newly acquired skills and knowledge in their home countries. The extent to which human capital transfer benefits the health sectors of source countries, however, is questionable when weighed against the negative effects of outmigration. While there are no reliable current statistics [72] on return rates of health workers, the extent of return migration is also believed to be limited [73]. Due to better income and employment prospects in other countries, many skilled health professionals seek to emigrate permanently.
The reality, thus, is that the large-scale outmigration of nurses often causes a brain drain with damaging effects on societies and healthcare systems. Labor migration often tears apart families [74], hampering the development of children [75], especially since migrant nurses are mostly females. Equally important, outmigration can exacerbate the shortage of nurses. In the English-speaking Caribbean, for example, health systems are in critical condition amidst a high outmigration of health workers. The World Bank estimated in 2009 [76] that three times as many nurses that were trained in the Caribbean region were working abroad than within the region. Jamaica’s Minister of Health noted in 2017 [77] that the brain drain of nurses has “virtually crippled the delivery of certain health care services and has had a dramatic effect on the overall quality of healthcare”. He added that the English-speaking Caribbean at large was facing a shortage of 10,000 nurses over the next ten years.
In the Philippines, 43,897 nurses [59] left the country between 2001 and 2004, whereas only 28,770 nurses passed the licensing exam and entered the labor market during the same time period. The Philippine Hospital Association reported in 2005 that 200 hospitals [68] had been closed and another 800 partially closed because of the outmigration of nurses. It should be noted, however, that the Philippines has since then produced an oversupply of nurses, and that inadequate nurse to population ratios are caused by a variety of factors beyond outmigration, including the underfunding of health systems and a lack of health facilities. The Manila Times reported in 2016 that there were 200,000 unemployed nurses [78] in the Philippines.
Impact on Education Systems
The example of the Philippines illustrates the impact large-scale labor migration can have on education systems. The establishment of a quasi-industrial nurse migration complex in the country has been accompanied by a mushrooming of mostly private nursing schools, pumping out nursing graduates by the tens of thousands annually at the expense of educational quality. Pass rates in the national nurse licensure examinations declined “from 85 percent in the 1970s and 1980s to only 45 percent to 54 percent between 2001 and 2004 [50]”, aided by the emergence of fly-by-night operators and schools offering “abbreviated evening and weekend programs tailored to physicians [50].” These developments have forced Philippine authorities to shut down increasing numbers of nursing schools. In 2013 alone, the country’s higher education commission closed 208 schools and programs [79], almost half of all institutions, because the pass rates of their graduates in licensing exams were below 30 percent.
Globally, the growing mobility of nurses has accelerated the harmonization and internationalization of nursing training, including an increase in transnational nursing education programs, offshore nursing schools, and bridging courses for foreign-trained nurses. U.S. students, for instance, can now prepare [80] for U.S. licensing exams at an offshore school [81]on the Caribbean island of St. Kitts, while the private Indian nursing education provider INSOL [82] promises to “transform Indian Nurses to Global Nurses” via post-RN graduate programs in six Western countries. In another example, several Australian and British universities offer a range of transnational nursing programs in countries like the Philippines [83] and Malaysia [84]. Governments worldwide, meanwhile, are increasingly shifting from hospital-based to university-based education models – a trend that facilitates mobility. In countries like the Ukraine or Hungary [85], the introduction of bachelor’s and master’s programs in nursing, which often incorporate an English-language component, has facilitated to outmigration of nurses.
At the same time, the strong export orientation of nursing education systems in countries like the Philippines can produce significant brain waste by keeping graduates dependent on cyclical fluctuations in labor demand. As the sociologist Yasmin Ortiga has noted, many Filipino nursing graduates have found themselves caught in a “migration trap [86]”: When overseas employment opportunities dried out due to declines in the demand for nurses in the U.S., scores of graduates lost their educational investments and ended up working in lower-skilled occupations.
The Need for Ethical Standards in the International Recruitment of Health Workers
The fact that the outmigration of nurses and other health workers tends to exacerbate health crises in developing countries raises moral questions about the recruitment of health workers in these countries by high-income nations. The headline-grabbing discovery of the body of a murdered Filipino domestic worker in a freezer in Kuwait [87], and the subsequent recall [88] of thousands of Filipino workers from Kuwait in February 2018, illustrates that migrant workers are also vulnerable to violence, abuse, and exploitation abroad, or to fall victim to scams by unscrupulous recruiters and criminals. It is therefore important that the migration and recruitment of health workers are as transparent as possible and governed by strong regulatory mechanisms in sending and receiving countries alike.
To this end, the 193 member countries of the WHO in 2011 adopted a “Global Code of Practice on the International Recruitment of Health Personnel [89]” that seeks to improve the management of health worker migration. While the code is non-binding and the degree of actual implementation in member countries varies, the agreement codifies important principles, such as equal legal rights and working conditions for foreign health workers, and the establishment of legal regulations for the international recruitment of these workers. It urges member states to increase the international coordination of labor migration and to adopt policies designed to “reduce their need to recruit migrant health personnel” in the first place. Also, the code also calls on governments to gather comprehensive data on health worker migration – a step that could go a long way towards the systematic study and increased public awareness of a growing global phenomenon.
1. [90] United Nations: World Population Ageing 2015 [21], New York 2013, p.28.
2. [91] Altorjai, Szilvia and Batlova, Jeanne Batalova: Immigrant Health-Care Workers in the United States [92], Migration Policy Institute, 2017.