Wilson Macha, Knowledge Analyst, WES
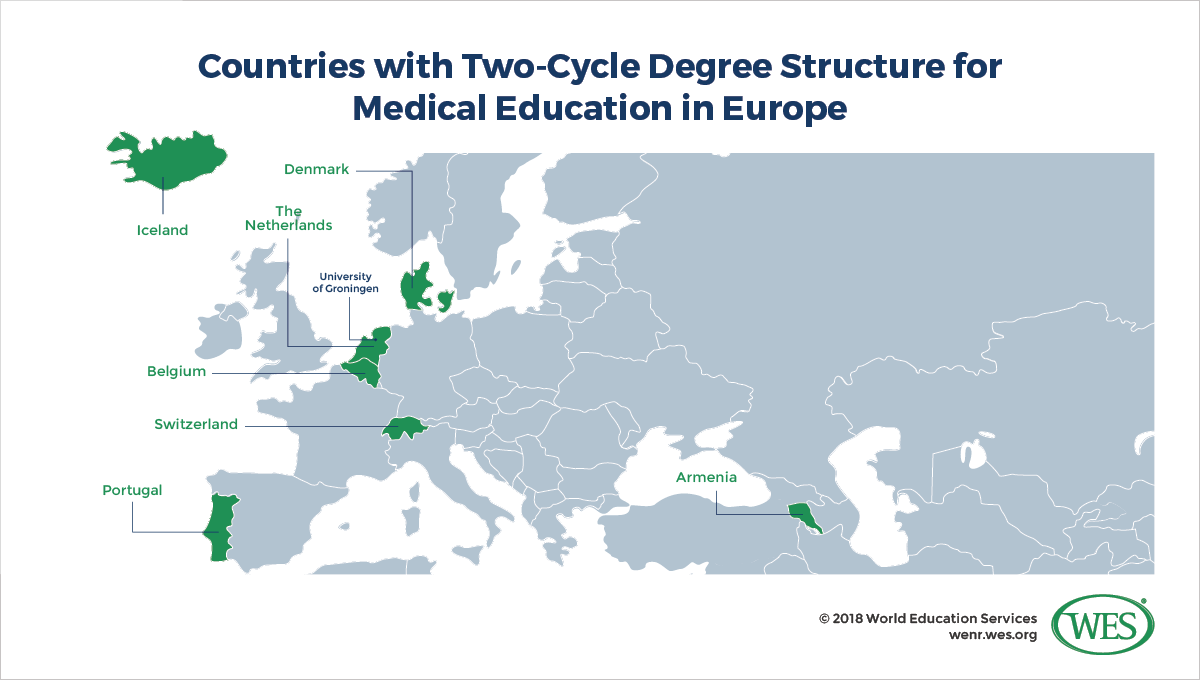
Since the 1999 launch of the European Higher Education Area (EHEA), most of the 48 states in which the Bologna Process is implemented have adopted a two-cycle bachelor-master degree structure similar to the British degree system. For regulated professions like medicine or dentistry, however, EHEA countries continue to offer first degree programs as unified long-cycle programs that are usually six years in length. Tallying medical education structures in all 48 countries, we found that only seven had adopted the bachelor-master structure in medical education.
That low number reflects the EHEA’s thin support for the two-cycle structure in medical education. From the outset, universities and medical practitioners fiercely opposed the splitting of medical education into separate bachelor and master programs. Some were concerned that the structure would lead to a deterioration of quality; others, that programs requiring six years of training would be split arbitrarily; and still others, that students would earn bachelor’s degrees of little use or relevance within the medical profession or other fields.
Is the two-cycle bachelor-master structure inherently incompatible with high-quality medical training? Not necessarily. The Association of Medical Schools in Europe noted in 2010 [2] that it did not fundamentally oppose adopting the two-cycle structure, as long as professional programs comprise “at least six years of study, or 5,500 hours of theoretical and practical training ….” be it delivered in unified programs or over the span of two degree cycles. This article provides a brief overview of the arguments for and against the two-cycle structure and discusses the reforms implemented at the Dutch University of Groningen as a potential model for two-cycle medical education in the EHEA.
Arguments Against Adopting the Two-Cycle Structure
Allan Cumming, a professor of medical education at the University of Edinburgh, summarizes [3] some of the main objections to dividing six-year medical programs into bachelor’s and master’s degrees:
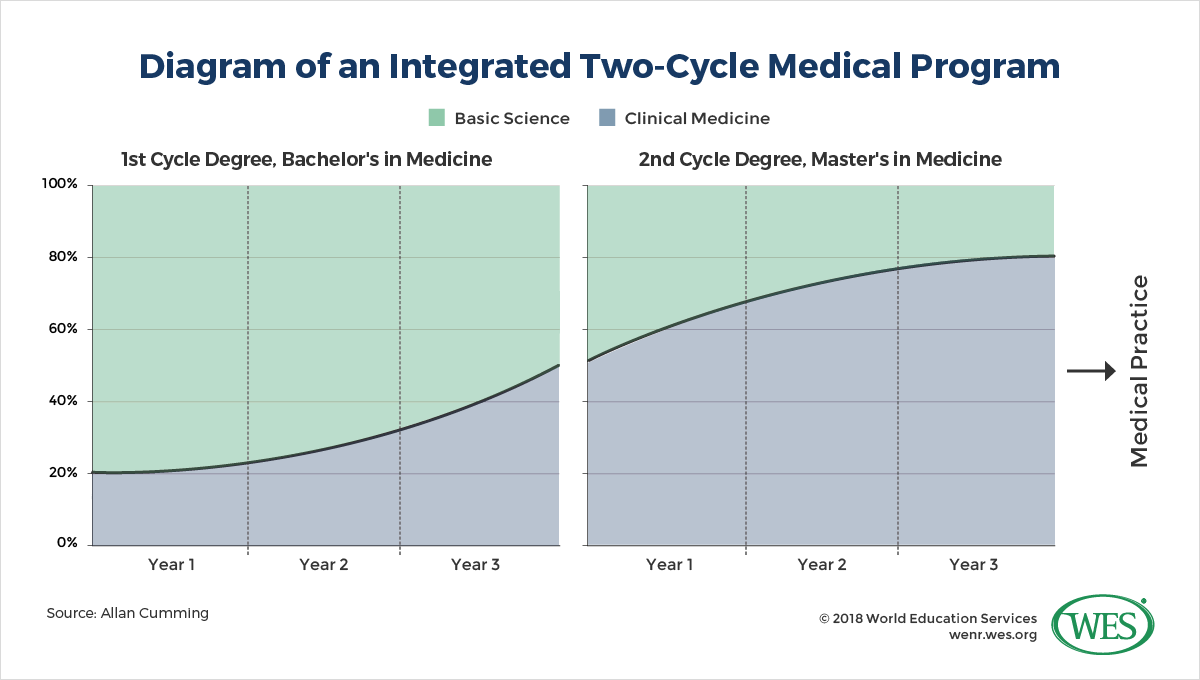
- The introduction of a three-year bachelor’s degree in medicine could have a disintegrative effect and result in “context-free basic science study” at the undergraduate level, “followed by a sudden switch to clinical medicine” at the graduate level. This could reverse recent efforts at European medical schools to create more integrated curricula, and perpetuate or even expand the so-called “Flexnerian model [4]”—a traditional approach to medical education that separates two years of initial premedical science studies from subsequent clinical studies. Still dominant in numerous countries, this model is now considered outdated by most European universities and is also increasingly questioned in the United States [5]. The integrated model currently pursued in Europe introduces both basic science and clinical medicine in the first semester and is thought to better engage and prepare students for further studies in a clinical environment.
- Long, unified medical programs are commonplace in many countries worldwide and are usually tightly regulated. Creating a separate structure in the EHEA would muddle the comparability of medical qualifications.
- The two-cycle structure would “create a large number of graduates with bachelor’s degrees in medicine, whose employment prospects and place in health care delivery systems would be unclear.”
This last point is stressed [6] by German medical professor Josef Pfeilschifter:
“What will the Bachelor of Medicine be qualified to do? She or he may have basic medical knowledge but is barely employable and cannot be let loose on the unsuspecting public anywhere in Europe. Indeed, the mandatory EU guideline … requires at least six years of theoretical and practical training to be eligible … as a practicing physician.… It has been argued that the Bachelor of Medicine might gain popularity among medical students, if they would take it as an opportunity to drift away into the non-curative branches of the field …. We argue that this is nonsense … why should we encourage our students to quit before they have reached their and indeed our goal?”
More broadly speaking, some observers doubt that pan-European curricular harmonization within the Bologna framework is in the best interests of patients and societies, since medical needs vary from country to country. For example, Professor Jan B.M. Kuks of the University of Groningen questions whether the current Dutch curriculum, which includes only limited training in obstetrics, would make sense in Kazakhstan, a country that has a fertility rate nearly twice that of the Netherlands [7].
There are also some concerns that the current emphasis on international mobility and English-language instruction doesn’t support a patient-centered approach, since it could steamroll over country-specific needs and—at worst—be life-threatening. In this view, effective communication with patients requires fluency in local languages and familiarity with indigenous colloquialisms, health beliefs, attitudes, and culture [8].
Arguments for the Two-Cycle Structure
Two-cycle medical training was pioneered in the Netherlands and Belgium. The first [9] European university to adopt the new model was the University of Groningen, which launched a bachelor-master structure in 2003, and in 2009 graduated the first students to earn a Master of Medicine degree. The other countries that have adopted two-cycle systems in medicine are Armenia, Denmark, Iceland, Portugal, and Switzerland.
The degree structures that universities in these countries adopted range from 3+3 to 4+2 models [10]; the degrees awarded may be a Bachelor of Science or simply a Bachelor of Medicine in the first cycle, as well as the Master of Science in Medicine, Master of Medicine, or Doctor of Medicine in the second cycle.
The few countries that have switched to two-cycle medical education use different models. While a select few initially kept their old curricula and issued “pro-forma” bachelor’s degrees or the so-called “bachelor en passant [6]” en route to completing a longer professional program, others undertook full-scale curricular reforms [10]. Institutions in the Netherlands and Switzerland, for example, have significantly modified their curricula to accommodate the new structure.
Surveyed about their experiences with these reforms, many universities reported challenges related to keeping curricula integrated across the two degree cycles. However, they also noted a number of discernible benefits, such as greater comparability of medical study and degrees (because of the standardization of ECTS credits), and increased opportunities for student mobility and the “possibility of building bridges between all health care systems [10].”
One forceful argument in favor of the two-cycle structure is that it affords students greater flexibility in switching academic careers. It gives those who decide midway into the program not to pursue a medical career, or who drop out for academic or other reasons, the chance to earn at least a bachelor’s degree. At the University of Groningen, it is also possible for bachelor’s degree holders in medicine-related fields like pharmacy, psychology, or physical therapy to enroll in medical master’s programs after they complete a one-year bridge program. [7]
Another argument in favor of the two-cycle approach is that standardizing medical education across Europe will enable a more robust Europe-wide quality assurance or accreditation system—although some have questioned whether pan-European accreditation of medical education is even viable in light of each country’s unique medical needs and the prior existence of national, discipline-specific accreditation mechanisms in the medical field. What works for Denmark may not work for Kazakhstan, and attempting to accredit programs in 48 countries using the same rubric is a tall order, although a European accreditation system already exits for medical specialties – the European Accreditation Council for CME (EACCME [11]).
Medical Education at the University of Groningen: A Model for the EHEA?
The University of Groningen shows that it may be possible to successfully implement two-cycle medical training without risking the disintegration of medical curricula. The university undertook an extensive review of its curriculum and reformed it, producing the G2010 [12] curriculum, which in 2014 was further reformed to the current G2020 curriculum [13]. Medical education at Groningen consists of a three-year bachelor’s degree (180 ECTS) and a three-year master’s degree (180 ECTS) – a structure that has since been adopted by all Dutch medical universities.
At Groningen, bachelor’s degrees are offered in four specializations: global health (an interdisciplinary program focusing on “disease in relation to political, social, and economic factors [14]”), sustainable care, intramural care, and molecular biology. In addition, all programs include the same basic medical education component. This is followed by clinical internships and hospital-based clinical training during the master’s phase [15].
To ensure that the bachelor’s degree is a viable stand-alone qualification that signifies the holder’s employability, the university developed a set of core competencies and learning outcomes based on the Canadian Medical Education Directives for Specialists [16]. These competencies include skills in communication, research, management, ethical and professional reflection, patient investigation, clinical problem-solving, and analysis of social and local context of medicine. Students are also required to write a thesis in the final semester of the program.
 [17]
[17]
While the bachelor component focuses primarily on basic sciences, the integrated Groningen curriculum emphasizes patient interaction from the first year of study and incorporates hospital internships as well as studies in clinical medicine, the amount of which increases over the course of the program [18]. An integrated program, the Groningen curriculum is not a return to the bifurcated flexnerian model.
On the face of it, the Groningen model is, in fact, more integrated than the standard medical curriculum in Germany, which is divided into two years of initial pre-clinical studies and a four-year segment of clinical studies [19].
To the careful reader, the difference between the integrated Dutch and the bifurcated German curriculum may be striking, but medical education in Germany has a long tradition that began in 1386 with the foundation of the University of Heidelberg, and any changes in the medical curriculum face an uphill battle. Though Germany seems entrenched in the flexnerian model of medical education, there have been some efforts, namely by the German Council of Science and Humanities [20], to introduce a more integrated approach.
Although Groningen’s bachelor graduates are not eligible to work as physicians, they do obtain the necessary fundamental science skills that all medical students need to acquire. They are also introduced to clinical settings, and upon graduation they are expected to be able to examine patients. Beyond their medical education, students receive broader academic training to enable them to apply medical knowledge in social settings. This broader academic exposure is intended to prepare them for employment in other health-related fields, as well as for further academic studies and scientific research.
Groningen’s G2010 curriculum seems to have successfully skirted the problem of disintegration, and the new G2020 continues that progress. While most clinical work is reserved for the master’s program, bachelor’s students are given time with patients in the form of interviews and tutor-led visits to medical clinics. And for those who decide not to pursue the master’s, a large portion of the bachelor’s program is focused on basic sciences and communication and critical thinking skills that equip those students to be competitive in the job market.
Conclusion
Converting current long-cycle medical degrees into the two-cycle structure would force many institutions to make changes to their curriculum and shift their priorities. For example, they would need to make certain that students who complete only the first cycle will still have viable career options and graduate having developed certain competencies.
However, Groningen’s competency-based, patient-centered curriculum shows that the two-cycle structure can remain integrated. The two-cycle structure has, for the most part, been accepted by Dutch society, even though the majority of Dutch medical students continue to complete the full six-year curriculum, so that the labor market value of a bachelor’s degree in medicine remains somewhat unproven.
Any pan-European medical curriculum must emphasize language and communication skills as well as critical problem-solving, as Groningen’s does. The communications needs of patients must drive any focus on the mobility of physicians. A curriculum that focuses on these skills works toward fulfilling the goals of the Bologna initiatives.
Most of Europe, however, opposes two-cycle medical education and medical students in most European countries have limited interest in an intermediate first cycle medical degree. Dr. Jadwiga Mirecka, in her guide [21] to the Bologna-style medical degree, concludes that the main problem medical schools have with the adoption of the two-cycle system is that its pros—“compatibility with other types of studies,” more career options, better mobility—do not outweigh the cons.
The future of European medical education is still unfolding and whether the two-cycle program will catch on remains to be seen. While the two-cycle degree places an emphasis on preparing students to be medically competent as well as adept in critical thinking and communication, the tradition of the long-cycle first degree is holding strong in European institutions. But the Dutch model certainly shows that there is a way to provide quality medical education within the two-cycle structure.